With mirrored RNA against highly aggressive brain tumors
 Universitätsklinikum Bonn
Universitätsklinikum Bonn
28. May 2024
Glioblastomas are particularly aggressive brain tumors that quickly grow into healthy brain tissue. As the tumors cannot usually be completely removed surgically, the prognosis for glioblastoma patients is very poor. Standard therapy - consisting of a combination of surgery, radiotherapy and chemotherapy - does not promise a cure. The search is therefore on for successful treatment options. Scientists at the University Medical Center Mannheim (UMM), the DKFZ-Hector Cancer Institute at the UMM and the University Hospital Bonn (UKB) led by Frank Giordano are researching a new therapy with a novel class of drugs consisting of mirrored RNA polymers, so-called Spiegelmers, which are designed to block the regeneration of glioblastoma.
In 2019, a study (GLORIA) was launched at six German university hospitals under the leadership of Mannheim to investigate how the active ingredient olaptesed pegol (NOX-A12,TME Pharma) works in combination with radiotherapy in glioblastoma patients for the first time.
"The special thing about our therapeutic approach is that we no longer focus solely on the radiation effects in tumor cells, but above all on their environment, the so-called tumor microenvironment. The Spiegelmer NOX-A12 prevents the formation of new blood vessels via a mechanism that is specifically stimulated by remaining tumor cells after radiotherapy in order to regenerate," explains Professor Dr. Frank Giordano, Director of the Department of Radiotherapy and Radiation Oncology at the UMM, who also conducts research at the DKFZ-Hector Cancer Institute.
Tumor cells are dependent on the supply of nutrients and oxygen in the blood. They therefore send out messenger substances that promote the formation of new blood vessels and encourage them to grow in the direction of the tumor and supply it with nutrients. Deadly brain tumors also try to regenerate in this way after therapy.
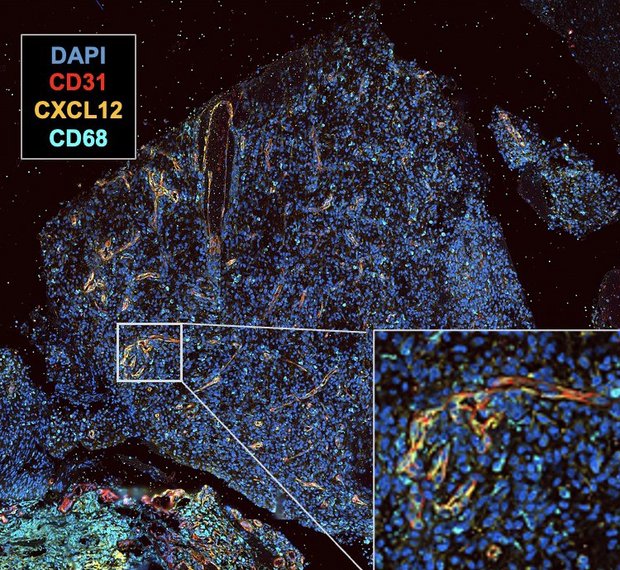
CXCL12 is one such endogenous messenger substance that stimulates vascularization. The Spiegelmer NOX-A12 inhibits CXCL12 and thus torpedoes the regeneration of the tumor. "It is interesting that the principle apparently only works in combination with radiotherapy, as glioblastomas use this repair mechanism via CXCL12 particularly after radiotherapy," emphasizes Professor Giordano.
In an initial phase I/II study, the new therapy was tested for the first time on a small group of patients with a newly diagnosed glioblastoma who are resistant to standard therapy. The main aim is to obtain information on the safety and initial indications of the efficacy of NOX-A12 in combination with radiotherapy.
In addition, the study also provided new findings that are important for the further development of NOX-A12 therapy. Under the direction of research groups at the University Hospital Bonn, tissue samples from the tumors were examined using state-of-the-art methods. "If the tumor cells and, interestingly, the vascular cells themselves produce a lot of CXCL12, this seems to correlate with a better response to NOX-A12 therapy," explains Professor Dr. Michael Hölzel, Director of the Institute of Experimental Oncology at the UKB, who also conducts research at the University of Bonn. "However, further studies and a larger number of samples are needed to really substantiate this observation," Professor Hölzel qualifies.
However, the initial data are already so promising that the US Food and Drug Administration (FDA) has not only approved the application for NOX-A12 as an investigational new drug (IND), but has also approved the application for fast-track designation, thus shortening a process that would otherwise take several years.
The university hospitals in Mannheim, Bonn, Essen, Münster, Tübingen and Leipzig are involved in the study. The results of the study have just been published in the renowned journal Nature Communications.