 Lisa-Marie Rieckmann, DKFZ-Hector Krebsinstitut an der UMM
Lisa-Marie Rieckmann, DKFZ-Hector Krebsinstitut an der UMM
Circulating tumor cells provide detailed insights into cancer heterogeneity
08. May 2024
An improved method for isolating circulating tumor cells paves the way for tailor-made therapies in personalized oncology: in a recent study, study leaders Sonja Loges and Melanie Janning from the DKFZ-Hector Cancer Institute at the University Medical Center Mannheim show that it is possible to obtain sufficient circulating tumor cells using a blood cell enrichment technique (diagnostic leukapheresis) to comprehensively analyze the tumor and its heterogeneity.
This is an important step towards personalized oncology: "In future, we will be able to gain deep insights into the response of each patient to their therapy in a minimally invasive way - using a blood sample," says Sonja Loges, who led the study together with Melanie Janning.
Leukapheresis is normally used in haematology to specifically filter leukocytes from the blood, for example to obtain blood stem cells for transplantation. The blood is separated into its components by centrifugation in a cell separator, white blood cells are selectively removed and the remaining blood components are returned to the patient.
Tumors are heterogeneous: they can differ from one another in different parts of the tumor. This phenomenon plays an important role in cancer research, as cellular and molecular differences within a tumor can have an impact on both diagnostics and the use of targeted therapies. Heterogeneity is a major reason for the development of resistance to therapies.
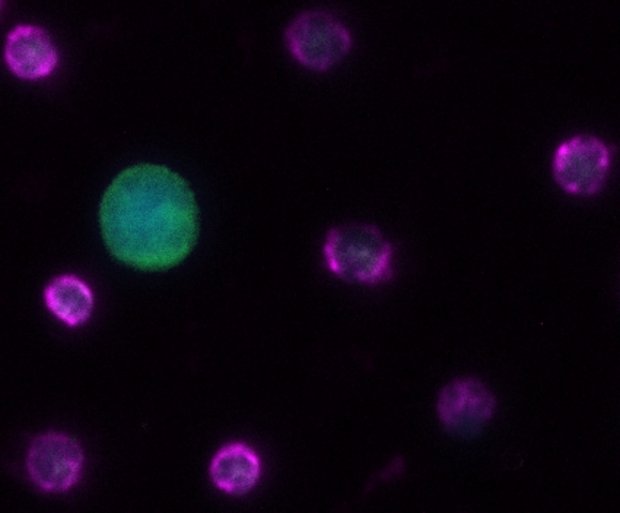
Tumor cells circulating in the blood (CTCs), potential precursors of metastases, represent a promising way of deciphering the heterogeneity of tumors. Like the analysis of tumor DNA circulating in the blood (ctDNA), the analysis of CTCs is a form of liquid biopsy in which the blood is examined for biomarkers. The method is used in cancer research and cancer diagnostics for various purposes: for screening and early detection of cancer, to assess the risk of metastasis, to identify target structures for therapy and resistance mechanisms, and for tumor monitoring.
However, the analysis of CTCs often reaches its limits because conventional methods for identifying CTCs often only provide very low cell counts, too low for a valid analysis of the tumor. This is also the case with non-small cell lung cancer (NSCLC). The scientists from the DKFZ-Hector Cancer Institute were able to overcome this limitation by developing an innovative two-stage procedure for the enrichment and isolation of CTCs. It is based on removing blood cells from the cell concentrate obtained during leukapheresis and thus subjecting larger volumes of patient blood to cell separation.
In the present study, this form of DLA was applied to six patients with advanced non-small cell lung cancer. The researchers succeeded in identifying an unprecedented total of more than 3,360 CTCs, which they were then able to analyze comprehensively. The results provided the researchers with unprecedented insights into cancer heterogeneity. The comparison of the active genes (based on the transcriptomes) of CTCs with those of primary NSCLC cells showed that the circulating tumor cells reflect the heterogeneity of their primary counterparts and at the same time exhibit unique CTC-specific characteristics.
"Due to the large number of CTCs available for analysis, we were not only able to confirm the diagnostic significance of circulating tumor cells in demonstrating tumor heterogeneity. We also succeeded in identifying potential CTC-specific signatures that can be used for targeted therapies in the future," says Lisa-Marie Rieckmann, one of the first authors of the study.
Melanie Janning, last author of the paper, adds: "This comprehensive method for characterizing circulating tumor cells represents a major advancement in cancer research. We are convinced that CTCs are a key element to better understand cancer dynamics. The methodology thus paves the way for tailored therapeutic interventions in personalized oncology."
The study was conducted in close collaboration between the DKFZ in Heidelberg and the University Medical Center Mannheim (UMM) as well as the University Medical Center Hamburg-Eppendorf and underlines the importance of interdisciplinary cooperation in the research of new cancer therapies.